Procedural sedation and analgesia (PSA) is the use of analgesic, sedative, and/or dissociative agents with the purpose of relieving pain and anxiety associated with a procedure.
It is well within the scope of the emergency physician and the aim of this post is to go over some key points as well as go over some of the most commonly used agents.
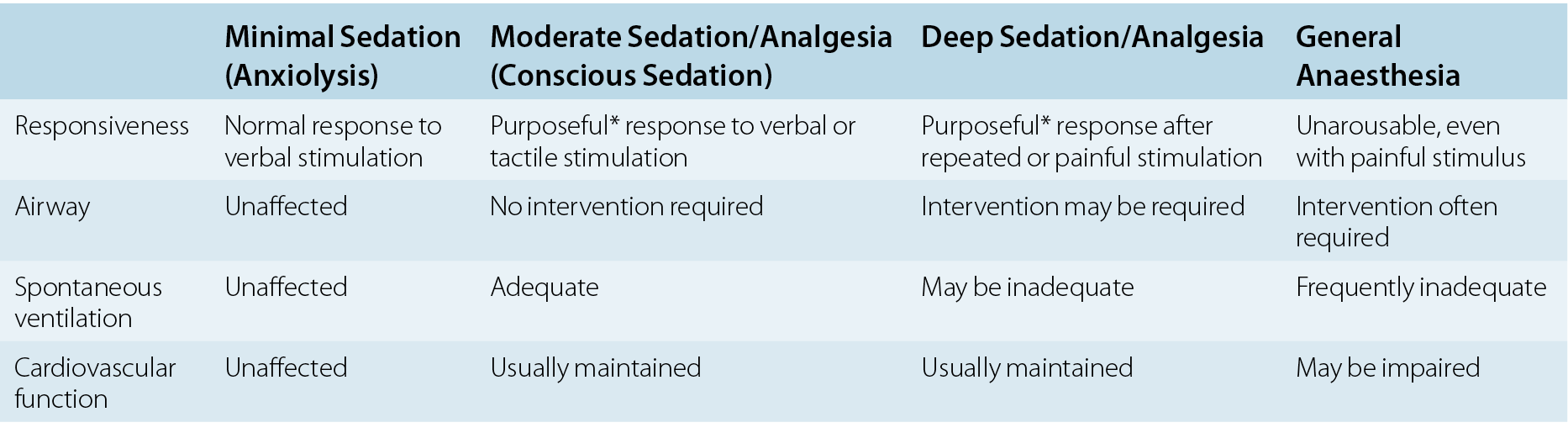
First thing to remember is that sedation is a spectrum and our goal state is determined by our indication for PSA including the duration of the procedure, and the level of pain/anxiety associated with the procedure.
We can then achieve our goal by careful selection of the proper agent, route, and dose.
Also take into account the patient’s age and comorbidities, including hepatic, renal, and cardiopulmonary insufficiencies.
For our purposes, PSA will only be referring to moderate sedation.
Our goal for PSA is to induce a state that allows a patient to tolerate unpleasant procedures while maintaining cardiorespiratory function by producing a depressed level of consciousness but allowing the patient to maintain airway control independently and consciously.
Before getting into the different agents, here are some definitions to be familiar with:
Analgesia: Relief of pain without intentional production of an altered mental state such as sedation. An altered mental state may be a secondary effect of medications administered for this purpose.
Anxiolysis: State of decreased apprehension concerning a particular situation in which there is no change in a patient’s level of awareness
Dissociation: Trancelike cataleptic state in which the cortical centers are prevented from receiving sensory stimuli, but cardiopulmonary activity and responses are preserved.
Can you guess which PSA agent was used on this pediatric patient?
Find out next time in our PSA POTD - Part 2!