This weeks VOTW is brought to you by Dr. Eng and Dr. Xu!
An 82 year old male presented to the ED w/ confusion, slurred speech and fall. A stroke alert was called initially, however the EKG obtained showed deep inverted T-waves in the anterior leads as well as ST-elevation in I and aVL. A POCUS was performed which showed…
Clip 1 shows a parasternal short axis view of the heart. The septum, posterior and inferior walls appear to be contracting appropriately but the anterior and lateral walls appear akinetic. Clip 2 shows an apical 4 chamber view of the heart where again the septum appears to be contracting well but the apex and lateral walls appear to be akinetic. The area of akinesis correlates with the ST-changes seen on the EKG.
SALPI
Regional Wall Motion Abnormality
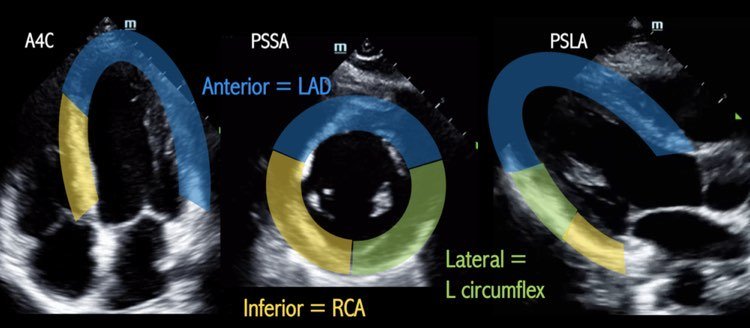
To evaluate for a regional wall motion abnormality (RWMA) remember the acronym SALPI (image 1). In the parasternal short axis view, starting at the septum, go clockwise to identify the anterior – lateral – posterior – inferior walls. To look for a RWMA, look closely at each wall during systole to see if:
The myocardium is moving in towards the center of the ventricle
The myocardium is increasing in thickness
The absence of these findings is concerning for a RWMA which may be indicative of an acute MI. Patients with old MIs may also have RWMAs - correlate with the EKG and old echos if available
The parasternal long axis view and apical 4 chamber views can also be used to evaluated for RWMA (image 2).
When to POCUS for RWMA
This may be especially helpful in patients w/ equivocal EKGs that you or cardiology is on the fence about activating the cath lab or when the symptoms are not quite consistent with an MI (as in this case). Finding a RWMA may expedite cath lab activation (1).
Pro Tip: Cover up the entire LV with your hand except the specific wall you’re looking at and look at each wall seperately.
Back to the patient
The patient did not have any active chest pain but the initial troponin returned at 27.
The patient was taken to the cath lab which showed triple vessel disease with 80% stenosis of mid-LAD, 95% stenosis of first diagonal, 95% stenosis of proximal circumflex. He was evaluated for CABG but ultimately chose medical therapy.
References:
(1) Xu C, Melendez A, Nguyen T, Ellenberg J, Anand A, Delgado J, et al. Point-of-care ultrasound may expedite diagnosis and revascularization of occult occlusive myocardial infarction. Am J Emerg Med. 2022;58:186–91.